Recurrence after Dupuytren’s contracture release is common, particularly following minimally invasive procedures. This article summarises a retrospective study examining whether adding radiotherapy shortly after contracture release can reduce the risk of recurrence. The findings suggest that post-interventional radiotherapy is safe, well tolerated, and may significantly lower re-contracture rates—especially when combined with needle aponeurotomy—highlighting a promising strategy to improve long-term outcomes while preserving the benefits of less invasive treatments.
What We Did
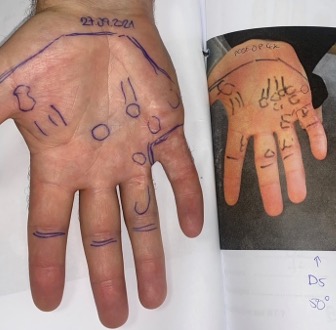
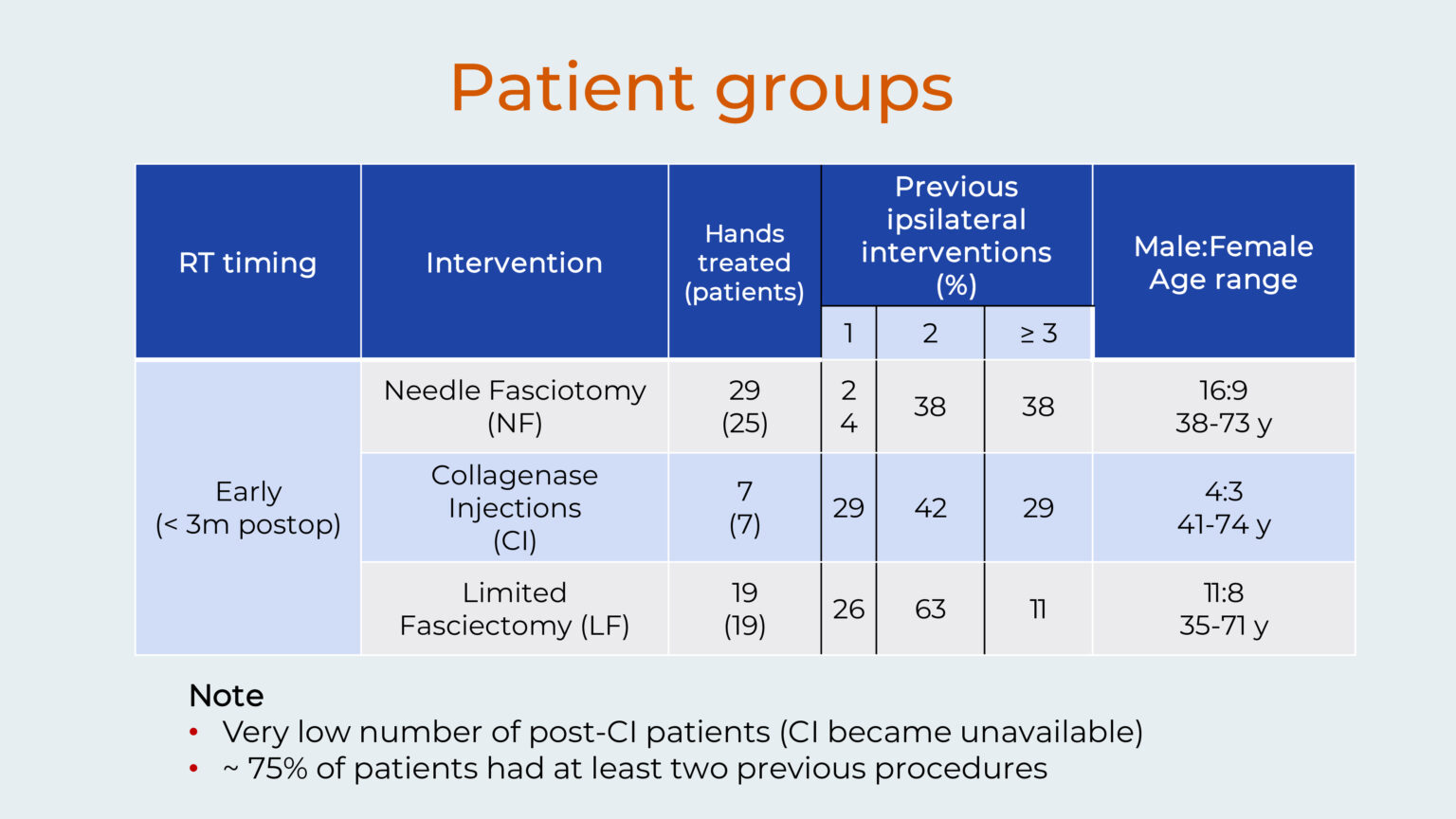
This retrospective study of radiotherapy given after contracture release was conducted by Dr Richard Shaffer and Professor Heinrich Seegenschmiedt. Fifty-one patients (55 hands) underwent contracture release using three different methods. These included needle fasciotomy (NF, 29 hands), collagenase injection (CI, 7 hands) and limited fasciectomy (LF, 19 hands).
The radiotherapy was always given within 3 months after contracture release. The patient population included more males, with ages ranging from 35-74 years. Importantly, about 75% of patients had undergone at least two previous procedures. Also, collagenase injection became unavailable during the follow-up period, resulting in a very low number of post-CI patients.
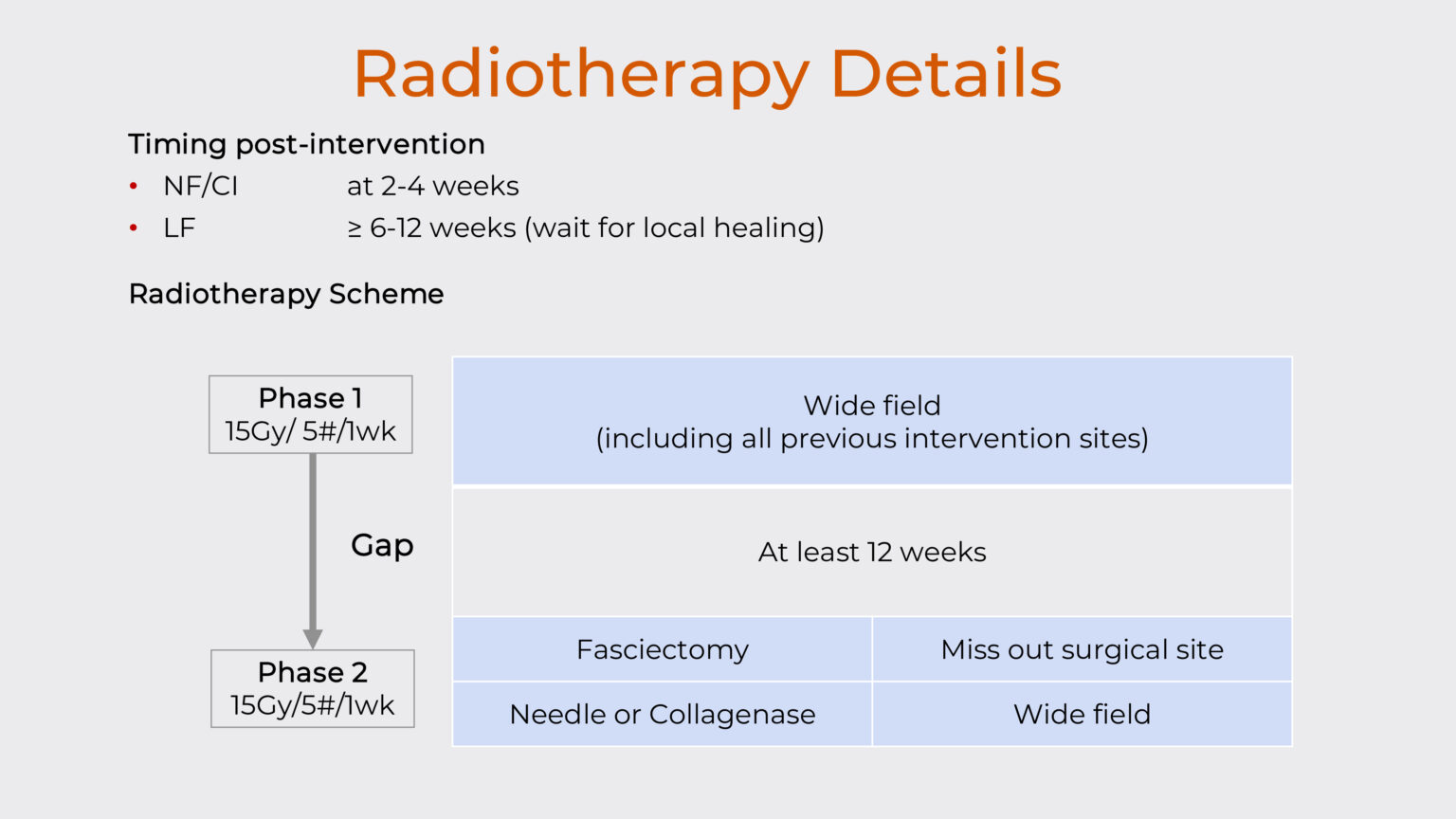
Post-operative radiotherapy was administered at 2-4 weeks after needle or collagenase and at 6-12 weeks after fasciectomy.
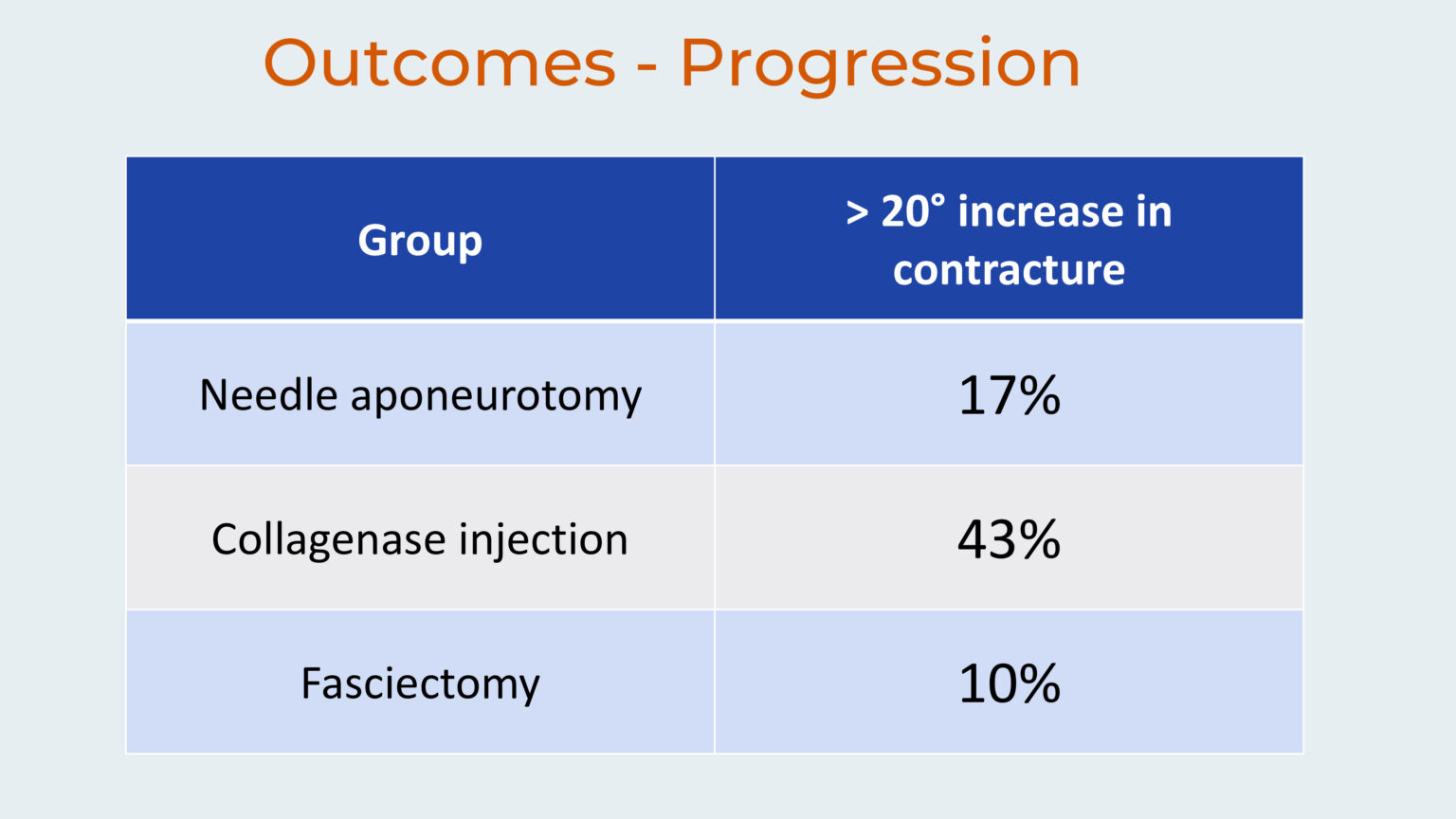
The primary outcome measure was defined as an increase of 20 degrees in the degree of contracture, and patients were followed for an average of 5.5 years, with all participants having a minimum follow-up period of one year. This study explores how we can improve the long-term success of Dupuytren’s disease treatment in the UK by combining radiotherapy with surgical release.
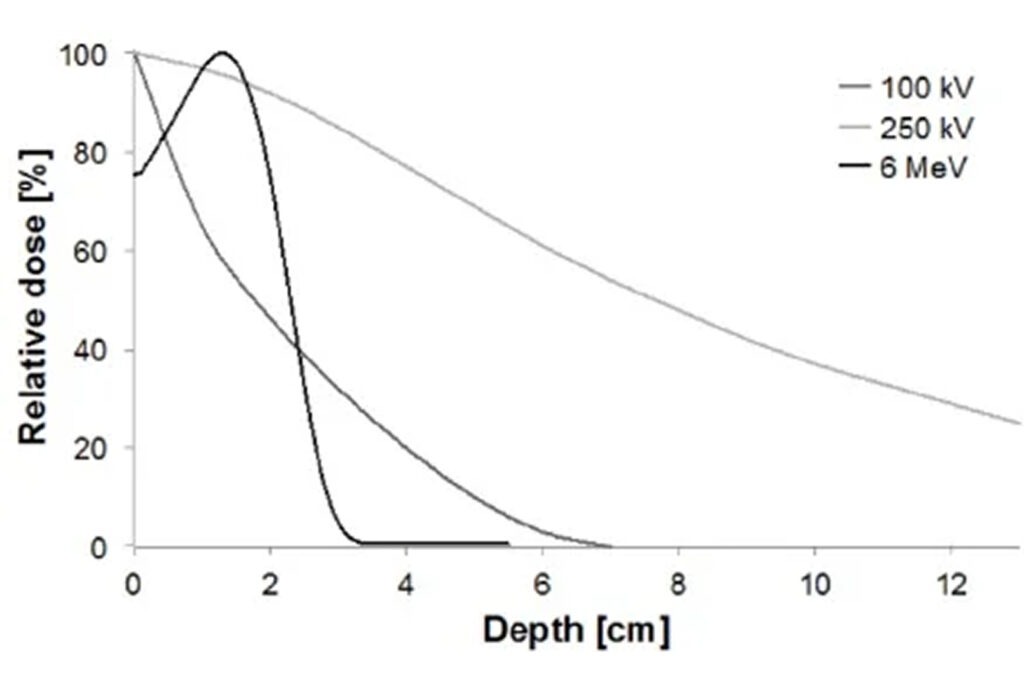
What Kind of Radiotherapy Was Used?
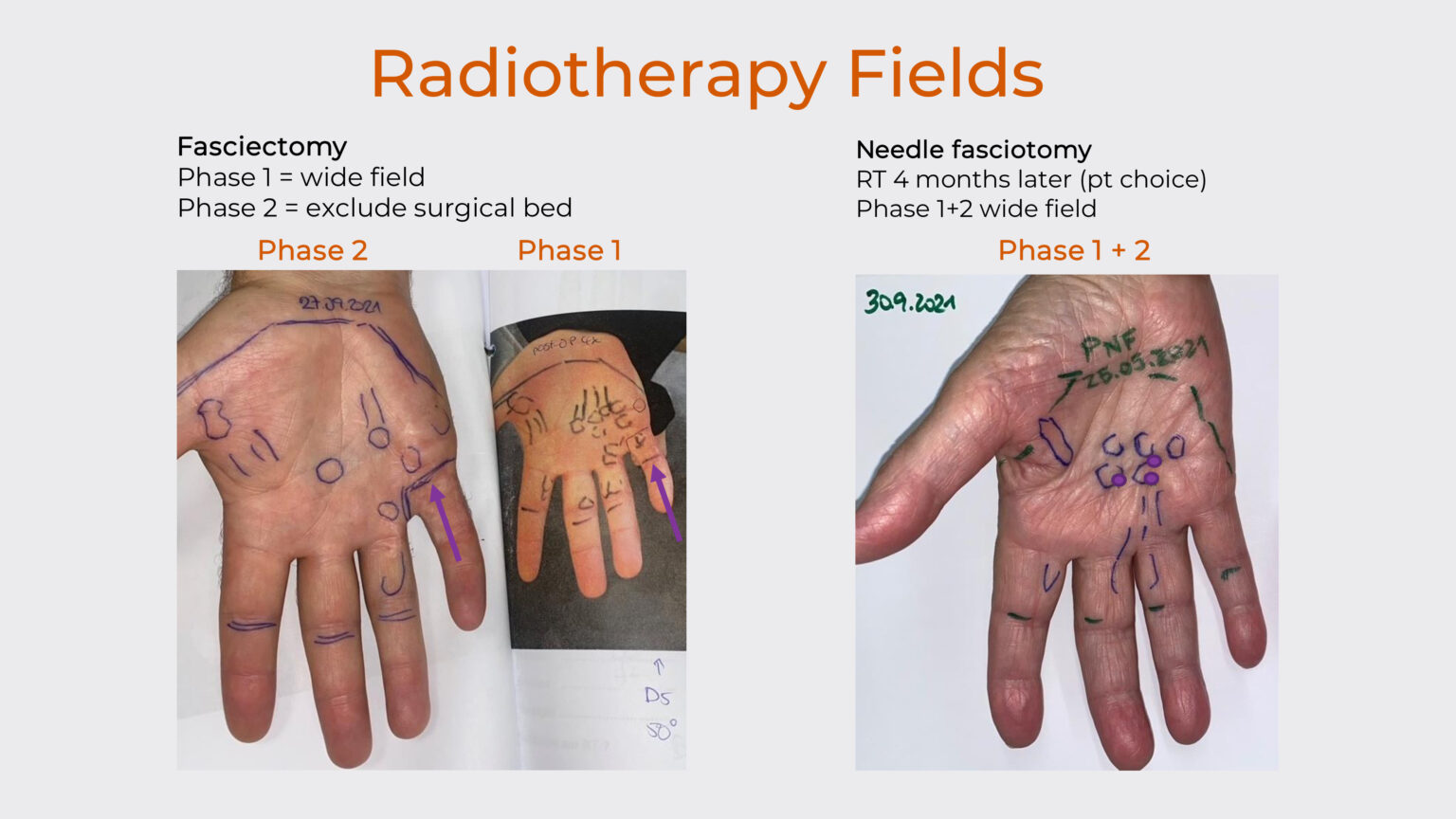
Each patient received treatment in two phases, with each phase consisting of 15 Gy in 5 fractions over 1 week, with a gap of at least 12 weeks between the phases to allow for tissue healing. The timing of starting radiotherapy varied by intervention type, with patients receiving needle fasciotomy or collagenase injection beginning treatment at 2-4 weeks after contracture release, while those undergoing fasciectomy waited 6-12 weeks to ensure adequate local healing before starting radiotherapy.
During phase 1, all patients received wide-field irradiation that included all previous intervention sites. Following the treatment gap, phase 2 delivery was tailored to the particular intervention: patients who had undergone needle fasciotomy or collagenase injection received the same wide-field treatment as in phase 1, while fasciectomy patients received a smaller treatment field that deliberately excluded the surgical bed to minimize complications at the healing surgical site.
Expert Non-Invasive Treatment for Dupuytren’s and Ledderhose Disease Across the UK
Dr Richard Shaffer set up Dupuytren’s UK in April 2011 to provide non-invasive treatments for people who suffer from benign conditions such as Ledderhose disease and early-stage Dupuytren’s contracture in the Guildford area. Today, Dupuytren’s UK offers this service to patients throughout the UK.
What Were the Results?
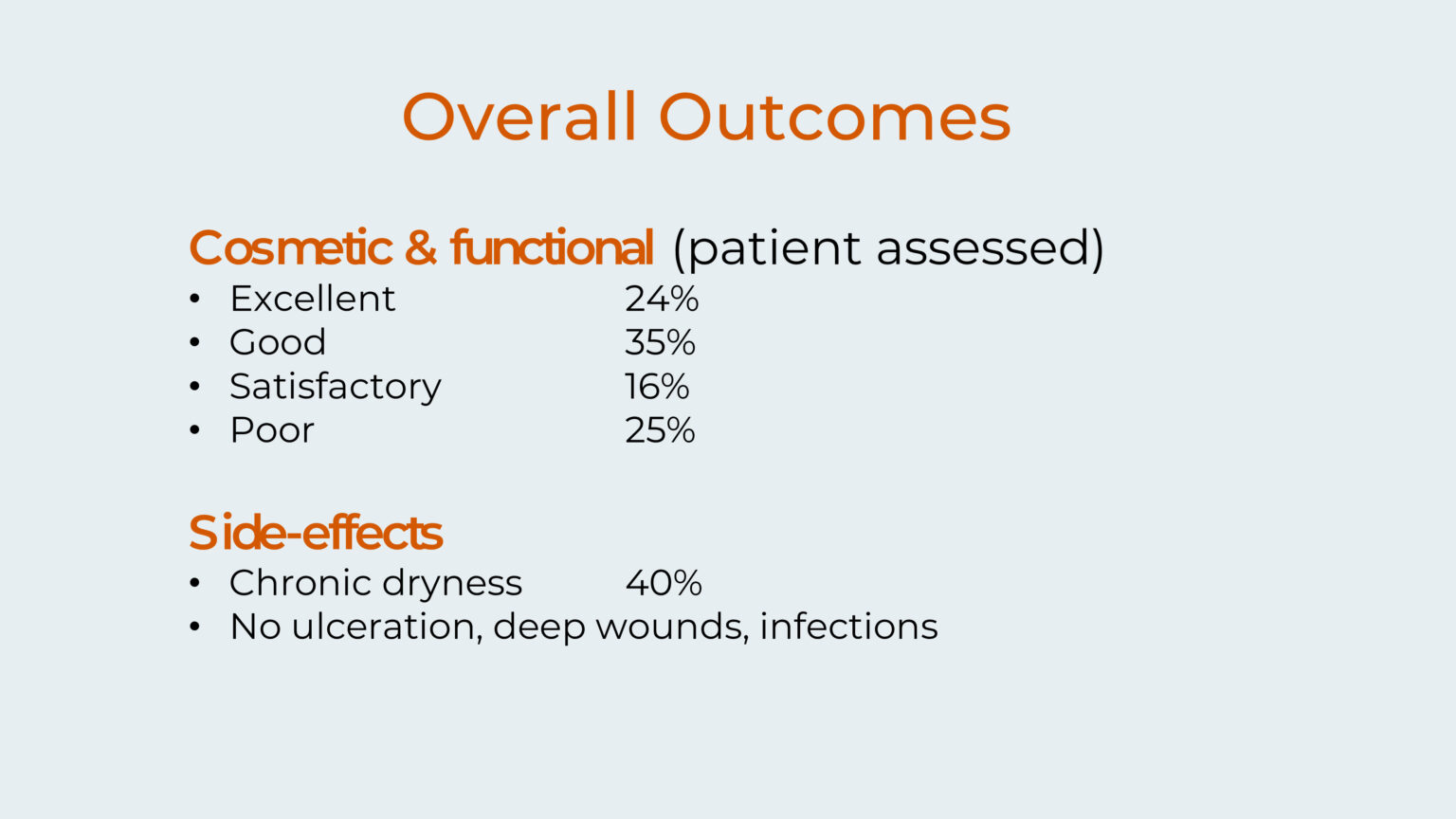
The results of the study showed promising outcomes for the treatment. When patients evaluated their cosmetic and functional results, 75% achieved at least satisfactory outcomes, with 24% rating their results as excellent, 35% as good, and 16% as satisfactory. Only 25% of patients reported poor results.
The treatment demonstrated a favourable safety profile, with side effects mainly being mild. The most common adverse effect was dryness of the skin, which affected 40% of patients. Notably, there were no serious complications. These findings suggest that the treatment offers an effective therapeutic option with manageable side effects.
Did the Contracture Come Back?
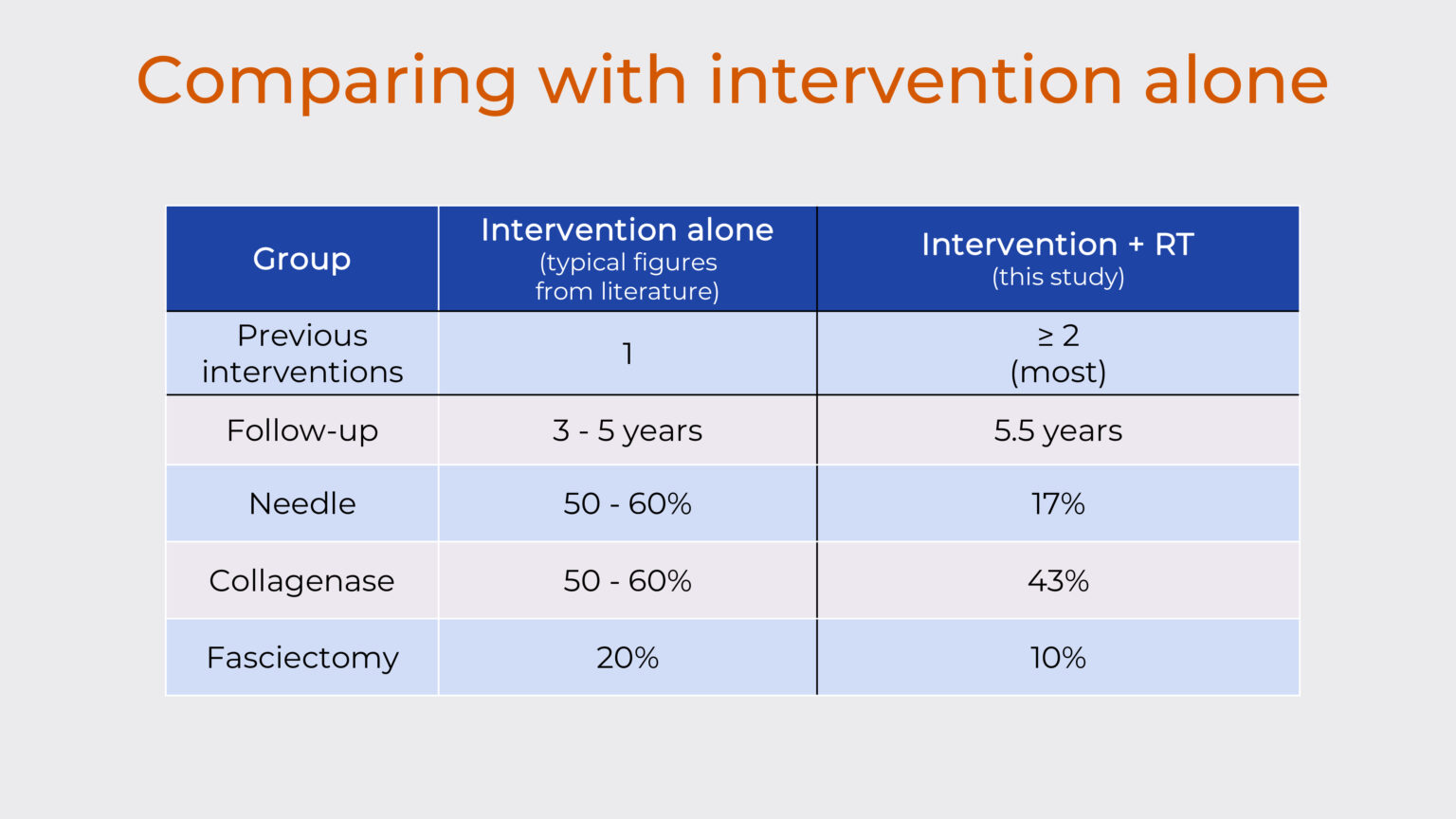
The combination of contracture release and radiotherapy treatment seems to give excellent outcomes. When you compare the results of this study with what you expect from contracture release alone you can see that the chance of the contracture coming back is much lower when you add in radiotherapy.
In particular, you would expect a re-contracture rate of 50-60% with needle alone, but when you add radiotherapy it is reduced to 17%. And with fasciectomy you would expect a recurrence rate of 20% and this is reduced to 10% when you add radiotherapy. Because of the low numbers of patients with collagenase, it’s more difficult to draw a conclusion about this part of the study.
Perhaps the most exciting aspect of this study is the combination of needle aponeurotomy with radiotherapy. This combines the advantages of a minimally invasive contracture release technique with the recurrence-reducing benefits of radiotherapy, offering patients an effective treatment option with significantly lower long-term failure rates than conventional standalone interventions.
What Does This Mean for Patients?
Based on the conclusions presented, this represents the first series of post-interventional radiotherapy for Dupuytren’s disease, demonstrating favourable outcomes when compared with typical published results of intervention alone.
This early study suggests that adding radiotherapy soon after a release procedure might reduce the risk of Dupuytren’s contracture recurring. However, this was conducted on a small patient group, without a comparison group and using historical literature as a benchmark.
More comprehensive research is needed to establish definitive conclusions and the medical community is currently awaiting results from the post-operative arm of the DEPART trial, which is a randomised controlled trial comparing radiotherapy versus no radiotherapy following intervention and is still recruiting patients in Australia and The Netherlands.
What Does This Mean for Patients?
Based on the conclusions presented, this represents the first series of post-interventional radiotherapy for Dupuytren’s disease, demonstrating favourable outcomes when compared with typical published results of intervention alone. The treatment approach proved to be safe, showing a similar safety profile to primary radiotherapy, while also achieving good patient-assessed outcomes. This early study suggests that adding radiotherapy soon after a release procedure might reduce the risk of Dupuytren’s contracture recurring. However, this was conducted on a small patient group and more comprehensive research is needed to establish definitive conclusions.
The medical community is currently awaiting definitive results from the adjuvant arm of the depart trial, which is a randomised controlled trial comparing radiotherapy versus no radiotherapy following intervention. If you’d like to know whether you’re a suitable candidate for this approach, further consultation would be advisable to assess your individual circumstances.