Dupuytren’s disease progresses differently for everyone, ranging from stable nodules that cause little trouble to tightening cords that bend the fingers and interfere with daily life. This comprehensive guide explains all current treatment options, from observation and hand therapy to radiotherapy, minimally invasive procedures, and surgery. It outlines when each approach is appropriate, the benefits and limitations of each, and why radiotherapy plays a unique role in slowing or stopping early-stage disease before contractures develop.
Dupuytren’s disease is a chronic condition in which the tissue beneath the skin on the palm thickens, forming lumps called nodules, which then form tight bands of tissue called cords. As the condition progresses, the cords may eventually bend one or more fingers, preventing full finger extension, so that the fingers are fixed in a bent position. This makes everyday actions such as gripping, typing, dressing, or handling objects more challenging. Many patients worry about how quickly it will progress and what the best treatment pathway might be.
Some individuals may develop a small lump (or nodule) in the palm that remains stable for many years, while others may develop a bend in one or more fingers (a Dupuytren contracture) as the tissue tightens over time. The speed and pattern of progression differ for everyone, which determines the choice of Dupuytren disease treatment. The choice you make will depend on the disease activity, the symptoms it is causing, and the treatment aims. Options range from simple observation all the way through to complex surgery, and each works differently.
The purpose of this article is to guide you through all currently available treatments. You will learn how each option works, its benefits and limitations, and the stage of disease for which it is intended. This includes a discussion about the use of radiotherapy, the only treatment that has been shown to slow or halt progression in the early stages of Dupuytren’s disease. Dupuytren’s UK specialises in low-dose radiotherapy for early disease and offers expert-led care for patients seeking a non-surgical approach.
Non-Surgical / Early-Stage Treatments
Non-surgical treatments are methods that do not involve incisions into the tissue or breaking apart the cords. Non-surgical options are used mostly in the early stages, when the aim is to reduce symptoms, slow disease progression, and avoid surgery. The initial signs in Dupuytren’s disease, as described by the NHS, are firm lumps (nodules) beneath the skin of the palm.
1. Watchful Waiting (Observation)
For some people, observation is a good option. This particularly applies to patients where it is very early, so where there are one or two nodules, where the disease has only been there for a couple of months or where it’s been completely stable for the last 6-12 months, and the fingers are still able to fully stretch backwards and have full span.
During this phase, you can observe for yourself how the disease progresses over time. If things remain stable, then no treatment is needed, but if the disease worsens over time, then you can consider radiotherapy treatment.
A full description of this option is found here, but in brief, you monitor the state of the disease every 1-2 months, paying attention to the following features.
- Number and size of nodules and cords on the palm and fingers
- Symptoms – pain/tenderness, tightness, itch, redness, increased prominence of nodules/cords
- Tighter fingers (see blog for how to measure)
- Reduced finger span (see blog)
If there is deterioration in these measures, then you should talk to your radiotherapy doctor to consider treatment.
2. Hand Therapy and Splinting
Hand therapy includes exercises to help preserve mobility and strengthen the hand. It’s important to keep the fingers mobile, but you should be careful not to overstretch the fingers too much, as this can cause trauma that may worsen the disease. Hand therapy cannot reverse a contracture or stop the disease from getting worse.
Splinting is also sometimes used to keep the fingers straight, but this requires wearing the splint in bed every night, which many patients find difficult. Also, once you stop using the splint, the contracture often returns very quickly.
3. Steroid Injections
Some patients are given steroid injections into the nodules. This is only really useful when the nodules are tender or inflamed and can give temporary relief from the tenderness. However, they are quite painful, and the benefits don’t tend to last for long. Also, repeated injections carry risks such as skin thinning or changes in skin colouration.
4. Biological injections
A trial in Oxford (the RIDD trial) tried out a drug injection called Adalimumab into the nodules. It found that the drug softened the nodules, but they didn’t assess whether it stopped the disease from getting worse or whether it reduced the formation of contractures. So it’s not clear whether this is useful for patients who want to avoid surgery. Also, the drug is not available for this use.
5. Shockwave treatment
The use of shockwave treatments may reduce pain in the nodules, but has not been shown to stop the disease from getting worse or prevent contractures or the need for surgery.
6. Other treatments
There are several other treatments that patients try, including anti-inflammatories, Verapamil cream, magnesium tablets, laser, ultrasound therapy, etc. You can see a full list here. However, none of these has good evidence supporting their use.
7. Radiation Therapy
Radiation therapy is an option in the early stages of Dupuytren’s disease, where there are nodules or cords on the palm or fingers. It is effective where there is either no contracture or a mild contracture of up to 20 degrees. Where there is a more advanced contracture (of 30 degrees or more), radiotherapy is not really effective.
The aim is to stabilise the condition so that it doesn’t get worse, so that it doesn’t form contractures, and so that you don’t need invasive surgery. It can also help relieve symptoms of tenderness or tightness in most people.
Why Radiotherapy Matters: The Dupuytren's UK Approach
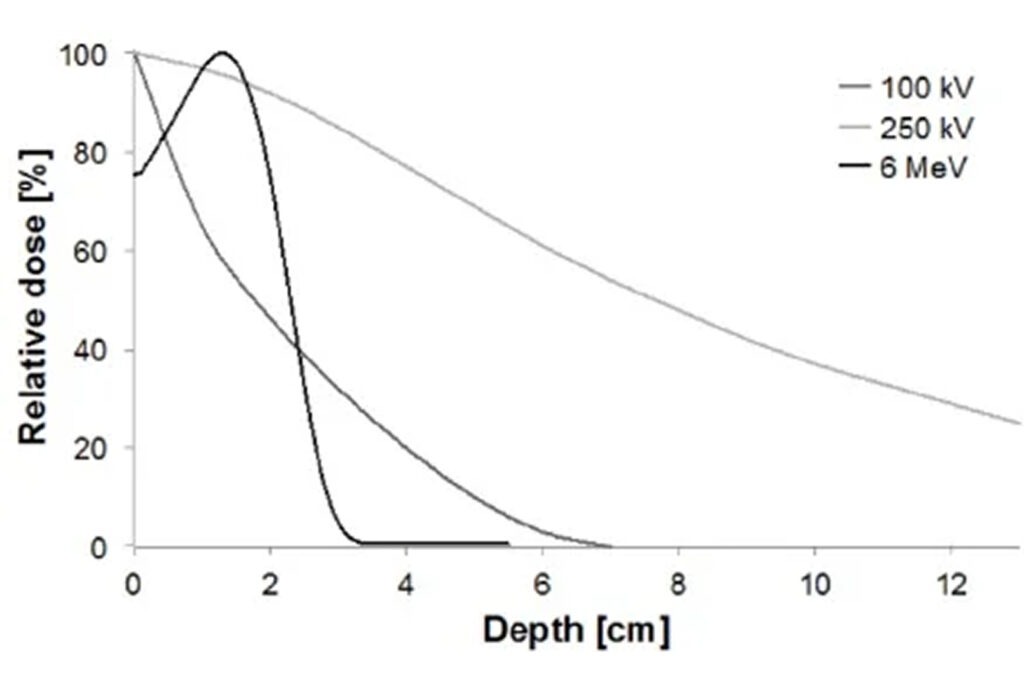
Radiotherapy for Dupuytren’s is very different from the high-dose treatment used to treat cancer. In Dupuytren’s disease, the doses are much lower (about half the dose) and are designed to modify biological activity rather than destroy tissue. Dupuytren’s UK is the leading clinic in the UK offering this treatment and has extensive experience in managing more than 3000 patients at this stage of the disease. The clinic treats patients with progressive nodules and cords, new areas of thickening or mild finger restriction.
Treatment for Dupuytren’s contracture is delivered in two phases:
- One 10-minute treatment each day for five days;
- Then a break of 3 months;
- Then a further five sessions.
This schedule balances effectiveness with long-term safety and is based on well-established European protocols.
Expert Non-Invasive Treatment for Dupuytren’s and Ledderhose Disease Across the UK
Dr Richard Shaffer set up Dupuytren’s UK in April 2011 to provide non-invasive treatments for people who suffer from benign conditions such as Ledderhose disease and early-stage Dupuytren’s contracture in the Guildford area. Today, Dupuytren’s UK offers this service to patients throughout the UK.
How Radiotherapy Works for Dupuytren's
The biological mechanism behind radiotherapy involves altering the behaviour of fibroblasts, the cells responsible for forming the scar tissue that forms the nodules and cords.
By reducing the activity of these fibroblasts and the inflammation signals in tissues, radiation therapy can stabilise tissue changes and prevent or reduce the formation of nodules and cords.
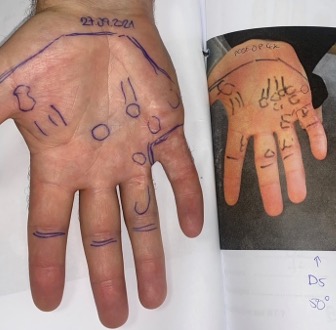
Treatment planning involves mapping the locations of nodules and cords to ensure the radiation field precisely targets all the affected tissue. This ensures maximum benefit while protecting healthy areas of the hand. Because each patient’s disease pattern is unique, custom targeting is essential to achieving optimal outcomes. You really need a radiation specialist who is very experienced in treating this condition to get the best results.
Minimally Invasive Treatments for Contractures
If you have a contracture of more than 30 degrees, then it’s too late for radiotherapy, and this is now a mechanical problem that needs a mechanical solution. Releasing a contracture can be done either with minimally invasive techniques or with more traditional surgical treatments.
Contracture release treatments for Dupuytren disease are used when the disease has progressed to the stage where the fingers are bent to more than 30 degrees and where the contracture is causing a functional problem for the patient. The aim is to straighten the finger by releasing the tight bands and straightening the affected joints. A detailed discussion about the benefits and risks with an experienced surgeon is crucial to understand the pros and cons of each option so that an individualised decision can be made.
Not every patient is eligible for minimally invasive treatments, and not every surgeon is able to offer the whole range of options. Generally, minimally invasive treatments are offered where the patient wishes to avoid surgical procedures and where the surgeon feels that they have a good chance of being effective.
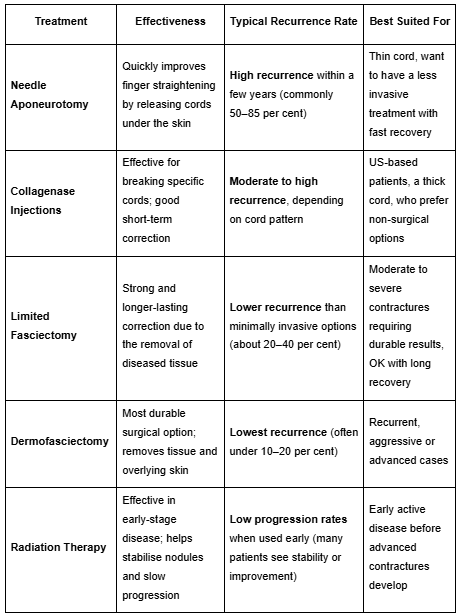
1. Needle Aponeurotomy (Needle Fasciotomy)
Needle aponeurotomy is performed by inserting a fine needle through the skin to release the tight tissue just beneath the skin. For this to be successful, patients need to have a relatively thin cord, as if the cord is very thickened, it tends not to be easy to release it with a needle alone. It’s a quick procedure that is done as an outpatient and doesn’t need a general anaesthetic. It’s ideal for people who prefer a quick procedure and rapid recovery – often patients get back to their normal activities after a day or two.
Unfortunately, recurrence is much more common with needle fasciotomy than with surgical options. There is, however, early evidence showing that giving radiotherapy a week or two after a needle fasciotomy can reduce the chance of the contracture coming back.
2. Enzyme Injection: Collagenase (Xiaflex)
An enzyme (collagenase) injection dissolves the cord that is tightening the finger. The most frequently used brand is Xiaflex (Xiapex). The injection softens the cord, and the doctor manipulates the finger around a day later to break the tight band. This approach has a short recovery time of around a week and avoids the need for incisions. Side effects include swelling, bruising or, rarely, tendon injury. Recurrence can happen, but the technique remains popular for suitable cases.
Unfortunately, this is only available in the US as it has been withdrawn from use in all other countries.
Surgical Treatments
Surgical treatments are recommended when contractures are severe or minimally invasive options are unlikely to be effective. Surgery provides a more complete excision of diseased tissue and may provide a more effective result. It tends to be done under general anaesthetic, but it’s also possible to have it done under local anaesthetic, using a WALANT (Wide Awake Local Anaesthesia No Tourniquet) technique.
Limited (Partial) Fasciectomy
Fasciectomy removes the thickened tissue through an incision in the palm and is done for moderate to severe contractures, and tends to have longer-lasting outcomes than the above minimally invasive options. It also requires a longer recovery period of around 6-8 weeks and carries typical surgical risks of wound complications, nerve injury, or stiffness. After surgery, it’s important to have a structured rehab plan, including post-operative hand therapy and splinting, in order to maintain finger extension and regain strength. Recurrence is possible, but at a lower rate than the less invasive techniques discussed, and this could be a reliable option when a more advanced condition is present.
Dermofasciectomy
Dermofasciectomy is a more involved procedure where both the diseased tissue and the overlying skin are removed. A skin graft is taken from the forearm and placed over the skin defect to cover the area. This is used for aggressive or recurrent disease, as it greatly reduces the risk of recurrence. The downside is a longer recovery. You also need carefully planned rehabilitation to avoid damage to the graft site and stop the contracture from recurring.
Comparing Treatments
1.Effectiveness vs Recurrence
2.Cost and Accessibility
Surgery is widely available in NHS and private settings. Minimally invasive options vary by region. Radiotherapy is accessible at specialist centres like Dupuytren’s UK and is covered by some insurance providers, including Bupa, Vitality, and WPA.
3.Recovery Time Comparison
For stabilising early disease, radiotherapy does not require downtime and is delivered gradually over months. For releasing contractures, minimally invasive treatments offer the quickest return to activities, whereas surgery requires a longer healing period.
How to Choose the Right Treatment
The best treatment depends mainly on the stage of your disease and how active it is. As a leading Consultant Clinical Oncologist, Dr Richard Shaffer has extensive experience in managing benign hand conditions using non-invasive techniques.
If you have early disease, the choice is between observation and radiotherapy. Getting seen early for a thorough assessment will enable you to understand how to actively observe your condition and what to watch out for to consider radiotherapy. It will also allow you to weigh up the pros and cons of radiotherapy when you consider this option to stop the condition from worsening over time.
If you have an advanced contracture of more than 30 degrees, then there are various options available to release the contracture. The choice is based on the availability of treatment options and your surgeon’s experience and expertise. They should discuss the effectiveness of each option for you in particular, taking into account how advanced the disease in your hand is and how it’s affecting your function. They should also discuss the pros and cons of each treatment so that you understand rehab and recovery time, as well as the various risks involved with each procedure. Meeting with a specialist will take all of these into account to advise you on a suitable treatment pathway. Through shared decision-making, as a patient, you are offered clarity about the benefits and limitations of each option before embarking on treatment.
If you have early-stage Dupuytren’s disease, book a consultation with Dupuytren’s UK today to discuss whether radiotherapy could help you.