Radiotherapy is most effective for early progressive Dupuytren’s disease, but not every early nodule needs immediate treatment. This article explains what “early” and “progressive” really mean in practice, why treating too soon can be unnecessary, and how patients can objectively monitor their hands over time. By using simple self-assessment methods such as photography, finger span, and hyperextension measurements, patients can identify true progression and choose the right moment to consider radiotherapy to prevent contracture.
Radiotherapy is effective in “early progressive disease”.
To explain what this means:
“Disease” means that there is a confirmed diagnosis of Dupuytren’s disease i.e. that you have nodules with or without cords and skin retraction (dimpling) and that this has been confirmed as Dupuytren’s disease by a suitably qualified and experienced doctor, for instance a radiation oncologist or a hand surgeon.
“Early” means that there is either:
No contracture i.e. no fixed forward bending of the fingers, Or early contracture (< 10 degrees).
There are certainly exceptions to this, for instance your radiation oncologist may offer you radiotherapy if you have a contracture of 10-20 degrees, with a careful conversation about the likely effectiveness.
“Progressive” means that things are getting worse, for instance:
- Nodules that are new or larger
- Cords that are new or larger
- Tightness of the fingers developing – see “loss of hyperextension” below
- New skin retraction (dimpling)

Reduction in finger span
At first glance, this “early progressive” definition could include patients with a new single nodule on their palm that appeared only a few weeks ago, and it is this group of patients that need to be cautious not to have treatment too early.
Sometimes people noticed the nodule a few weeks ago, but when they are examined by an experienced physician it turns out that they have further disease that they never noticed, or have a reduction in function (e.g. reduction in span or in hyperextension which is the ability to bend the fingers backwards), so that almost by definition they have had worsening, but they didn’t notice.
It may be that this is truly a single nodule, and the course of these is unpredictable. Often they may stabilise or regress and it is important not to treat these new single nodules with radiotherapy as it may be an over-treatment, or at least would have been given too early. In this case, patients must be given information on how to follow the course of their disease so that they know what to look out for and are empowered to return to the radiation oncologist when there has been true progression. If you’re at the right stage for treatment, you can find a detailed breakdown of what happens after radiotherapy in our post-care guide.
Expert Non-Invasive Treatment for Dupuytren’s and Ledderhose Disease Across the UK
Dr Richard Shaffer set up Dupuytren’s UK in April 2011 to provide non-invasive treatments for people who suffer from benign conditions such as Ledderhose disease and early-stage Dupuytren’s contracture in the Guildford area. Today, Dupuytren’s UK offers this service to patients throughout the UK.
Performing a test
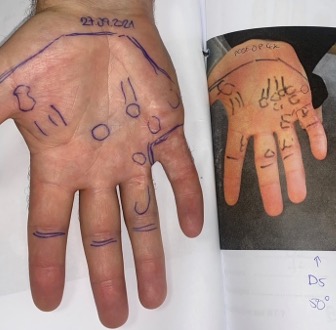
1. Photography
Draw around the nodules and cords with a felt-tip pen and take a photo with a ruler by it. This will be the baseline for the extent of the disease.

2. Hyperextension
Put your hand on a table top, press down on the first knuckle of each finger (see downward arrow in picture) and see how far the finger can be raised from the surface. Measure the distance between the finger tip and the table. This is the baseline for hyperextension. If this distance is reduced over time then you have developed “loss of hyperextension”.

3. Finger span
Put your hand on a piece of paper, extend your fingers outwards as much as you can so 3hat you are reaching as wide a distance as possible and then draw around the fingers. You can also take measurements between various fingers e.g. tip of thumb to tip of little finger, or thumb to index finger etc.

These tests can be repeated and carefully documented every month. If there is a significant change then you will have demonstrated “progression” and it may be the right time to consider radiotherapy to prevent further progression and contracture.
Summary:
Some patients should wait to be treated rather than plunging into treatment that may be costly, take up time, and could have side-effects. The tests above will empower you to objectively measure whether there has been worsening of your disease and therefore whether it is the right time to consider radiotherapy for early progressive Dupuytren’s disease.